Follicle Stimulating Hormone and Empty Follicle Syndrome
- Serena Caunce
- Jan 1, 2021
- 5 min read
If you’ve been following along in my blog, you probably have learnt that I did my Master’s research in reproduction. We used a lot of follicle stimulating hormone (FSH) in all of our protocols, whether we were collecting oocytes for IVF (in vitro fertilization) or for oocyte quality parameters (oocyte competence). We collected mature and immature oocytes. We collected from cattle and bison in the projects I worked on.
So, let's take a look at the steps that are required for oocyte collection. A transvaginal ultrasound probe is inserted to the vaginal fornix - this is the region surrounding the cervix. You can then see the ovary, with its follicles on the ultrasound machine. In cattle, we are able to hold those ovaries in our hand per rectum (as you would if you were doing pregnancy checks in cattle). You can hold that ovary, feel it, turn it, roll it, and position it so that we can collect the oocytes. In humans, this is not possible - adding to the difficulty for ultrasound guided follicular aspiration in people versus cattle and bison. On the ultrasound probe there is a needle guide, a long thin tube that fits a needle that is attached to some silicone tubing, which is attached to a filter system on the other end. Again, in cattle, while holding on to the ovary with our non-dominant hand, we take the needle and insert it into a follicle using our dominant hand (that's the hand you write with). We use suction with a vacuum pump to empty the follicle, then we turn the needle slightly so that the bevel of the needle scoops the inside of the follicle as it drains allowing the oocyte to be scraped from the inside of the follicle and suck down with the follicular fluid onto a filter. We then take this to the laboratory and rinse the filter into a petri dish, and do our searching for oocytes.
As researchers, when we troubleshoot why we didn‘t collect 100% of the eggs, it varies with the experience of the practitioner - how many animals have you collected? It can vary with the size of the bevel (short bevelled needles collect better than long bevelled needles). It varies with the amount of suction (to be honest, I forget the exact amount of vacuum suction). It is not because there is no egg. It is a function of technique, the skill of the practitioner, the pressure of the suction applied on the machine, or syringe if you are doing single aspirations, and perhaps over maturation and death of the oocyte prior to aspiration.
Empty Follicle Syndrome
What is Empty Follicle Syndrome? This is when no egg has been collected during egg retrieval when a women is undergoing IVF treatment. Even in the medical community it is under debate. It seems rare (<2% of women under going IVF, with women who have low AMH and low AFC being over-represented within that <2% affected).
There is also something called False Empty Follicle Syndrome (Kim and Jee, 2012). These women did not receive the appropriate dose of hCG for their 'trigger shot' or the oocytes were collected too soon after the hCG administration. The oocyte is there, but it was not retrieved. This could be due to failure of expansion of the cumulus-oocyte-complex (COC).
Ok, you need more details on what the COC is. Prior to the LH peak, the support cells called cumulus cells are tightly surrounding the oocyte and we call this a compact COC.
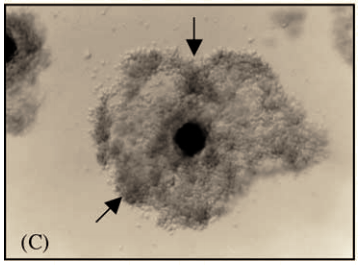
After the LH peak and prior to ovulation, these cumulus cells spread out and become sticky - we call this expansion. You have to have expansion of the cumulus cells, a sign of maturation of the oocyte in order to have fertilization. (Photos below from Ratto et al 2005 - (C) Partial expanded COC from llama; (D) Fully expanded COC from llama).
Note that this is a continuum from compacted to fully expanded, with the clumps of cumulus cells showing up darker, then spreading out into an even and lighter group of cells.
Expanded COC are sticky. The sticky cumulus cells help the oocyte travel in the female's fallopian tube (oviduct) towards the uterus. In human IVF, the majority of COCs undergo in vivo maturation and expansion following a 'trigger shot'. Hopefully that helps clarify things!
During follicular aspiration (also called OPU or ovum pick-up) the oocytes may or may not be mature, and the cumulus cells may or may not be expanded. Sometimes we get oocytes with no cumulus cells, which we categorize in a separate category - denuded.
It bothers me when people say and believe that not every follicle contains an egg (or oocyte). These are words that my RE has spoken to me, and the mean nurse (as described in a previous post) repeated it. I just do not believe it. I think in a normal follicle, each contains an egg. You can over-stimulate, and get oocyte apoptosis from oxidative stress. You can also have apoptosis from FSH starvation (see the image below). But prior to over-stimulation or 'coasting' protocols, you have an egg! So I really do not believe when someone says that not every follicle has an egg.
Histologically, if you take the ovary with its follicles, preserve it and slice it into tiny slices and look at it under the microscope, you will see that each follicle has an oocyte associated with this.
The truth is, you will not always retrieve 100% of the oocytes! Many doctors are Type A, high achievers, and they do not want to fail. Failure is less than 100%. So why set yourself up for failure?
FSH Stimulation Protocols in cattle
In our research lab, we have done a lot of studies on a short or standard FSH protocol of 4 days, and a longer FSH protocol of 7 days. The time from LH peak to oocyte collection (or AI for timed insemination protocols) is an important variable (we usually used GnRH as our injection for maturation - or trigger shot).
Prolonging the duration of FSH stimulation from 4 days to 7 days improves the oocyte quality after collection. Stopping FSH injections for a prolonged during prior to LH peak reduced the oocyte competence (the ability for the oocyte to become fertilized) (Dias et al, 2013).
Remember that cattle can be used as a model for human reproduction because clinical trials can be performed with more control over outside factors.
Gonal-f Pen
I started FSH stimulation on day 5 of my predicted cycle after estrace (estradiol) suppression. The Gonal-f pen came in a total of 900iu. The concentration ends up being 66ug/1.5mL. So if I am taking 150iu in the evening, this works out to be 11ug per dose.
As previously mentioned, I had an AFC of 2, grew 3 follicles total, and then had 2 follicles that were 13mm. I was not on an antagonist, and therefore, started to ovulate on my own. In our cattle protocols, were would use an intra-vaginal progesterone releasing device (called a CIDR) to suppress LH release. Sadly, I was not able to go ahead with the IUI and had yet another failed cycle.
It's my first post for 2021! This past year has seen so many struggles. So wishing everyone health and happiness for this up-coming year!









Comments